Latest Features
Are Oxygen Rebreathers Useful Tools for Tekkies and Sci-divers?
Mixed gas closed circuit and semi-closed circuit rebreathers have become essential tools for technical and scientific divers. But what about their pure oxygen counterparts? Diving contractor, scientist, and inventor Michael Lombardi believes that the time for O2 rebreathers’ may have come—not just for shallow water (≤10 m/33 ft) diving—shades of Hans Haas—but potentially to introduce motivated bubblers to CCR with a simpler rebreather.
by Michael Lombardi. Images courtesy of M. Lombard
A completely fortuitous venture resulted in spending more time on a rebreather than I had in 20 years of rebreather diving, though it wasn’t in the deep/wreck/cave environments often associated with the technology. It was very, very shallow and with nothing but oxygen, offering insights into what may be an overlooked opportunity: introducing rebreathers to a broader market.
Enter Rebreather Day 1.®
History & Context
In 2017, for-hire diving projects here in Rhode Island slowed a bit, and a colleague suggested commercially harvesting clams—or ‘quahogs’—to fill in some downtime. So, that’s what I did. It’s big business here in the Ocean State and an amazing fishery. The routine is to dive three to five hours per day to limit out. It’s all very shallow (6 m/20 ft or less) and most harvest divers use open circuit, though some use hookah. I started out diving 3-4 Aluminum 80s (AL80) per day. The first issue surfacing was that every time I switched out bottles, I would lose my place in the bed from it backfilling where I had cleared the mud out. So, I switched to two LP112s per day. That helped, but was destroying my back. Eureka moment—I can do this on a rebreather!
As a working diver, I always viewed rebreathers as a tool for the job. As of 2017, the only rebreather remaining in my dive locker was a 100% custom unit purpose-built for more technical interventions. It was far too much for harvesting, and far, far from the key element of being able to roll out of bed and go—everyday. So I put my developer hat on and took to the bench.
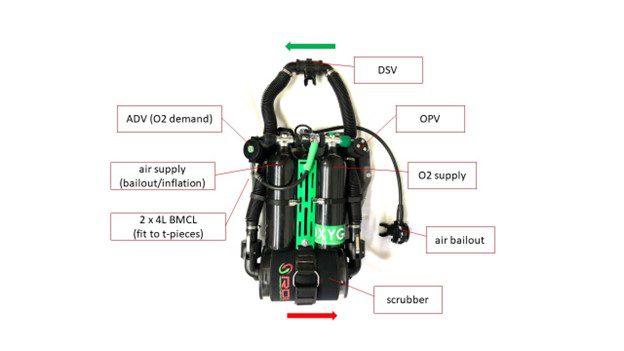
The task at hand called for specific criteria—a rugged system that could take the abuse of day-to-day work, back-mounted to keep my front clear since I was working close to the bottom, consumables for five hours, and enough bailout for the short return to the beach. Oxygen was supplied on-demand via a de-tuned ADV T-piece (an addition valve, rather than auto diluent valve). I designed/built two units that met the criteria and went to work. And I made a huge discovery.
I was able to dive all day, literally every day, on a rebreather—all with very low maintenance and turnover time and, most importantly, no chronic tinkering. Just get up and go diving, all while being more productive and arguably safer than on open circuit (OC) for the nature of the dives.

Since this 2017 inception, I’ve started to rethink my rebreather diving—so much so that I branded the unit “Rebreather Day 1®,” or RD1 for short, given my new belief that oxygen-only rebreathers might be an overlooked and alternate pathway to broader/early career market acceptance.
Spending multiple hundreds of hours with the original RD1 units has given me pause with the mainstream deep/wreck/cave paradigm mindset. These more ‘extreme’ experiences have been the way to lure in new rebreather divers, which is important, but remains volume-limited, given various barriers to entry: cost, training, proficiency, and perhaps most importantly perceived complexity. Mixed-gas rebreathers are still unattainable from a mass market standpoint for these reasons. Oxygen rebreathers arguably make these barriers easier to contend with and may be the early introduction needed to shift diving to a rebreather mindset.
Operational Techniques
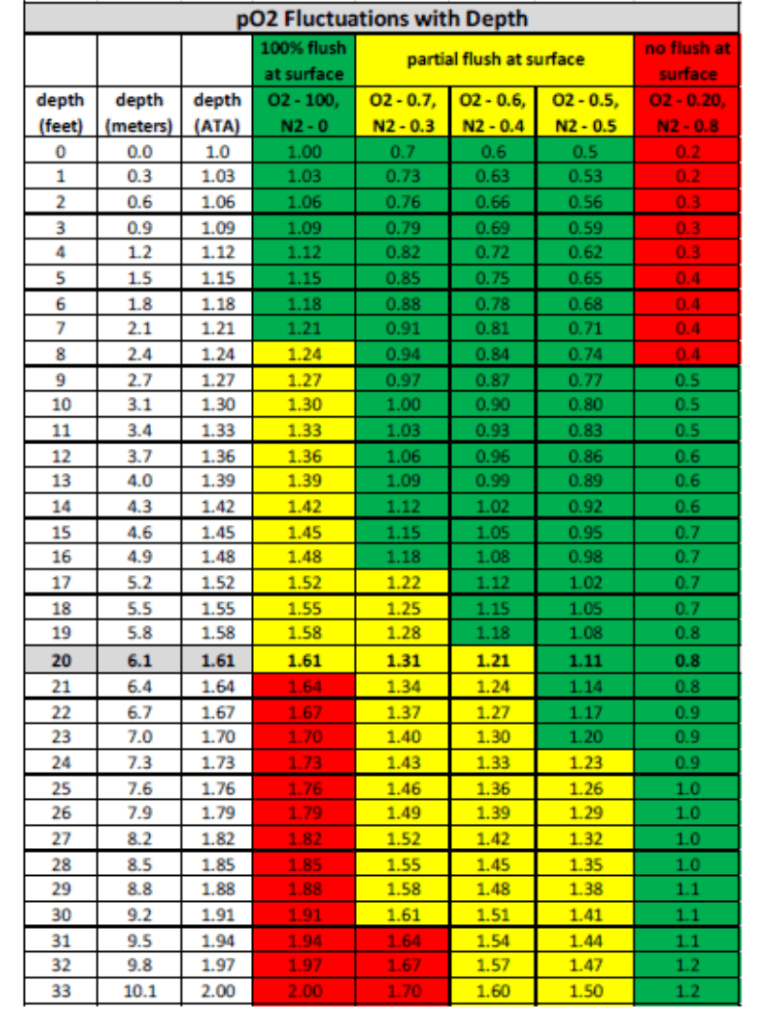
Now of course, oxygen rebreathers aren’t voodoo diving science. Oxygen rebreathers predate even open circuit scuba, let alone modern mixed gas rebreathers. There is an ill-informed assumption that the dives are limited to just 45 minutes due to 1.6 bar pO2 exposure (at 6 msw/20 fsw). This stems from being historically unable to monitor these circuits in the olden days.
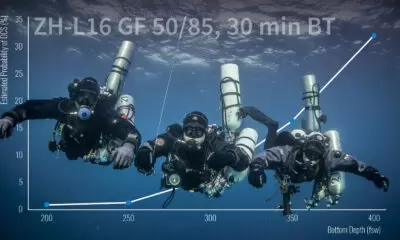
Today, fitting a monitor to an O2 rebreather reveals that it’s quite difficult to reach 1.6 bar given residual nitrogen in the lungs at the surface and, with advanced understanding of pre-dive loop flushing (easy to teach), it’s not terribly difficult to maintain lower PO2s and enjoy lengthy dives, even up to 2 ATA depth.
One operational practice I’ve adopted while diving manual closed circuit rebreathers (mCCR) is riding a PO2 ‘bubble’ +/- 1.0 bar throughout the dive. It keeps on-the-fly math easy and doesn’t extend decompression too significantly versus riding a higher fixed pO2. I’ve always felt that we have no shortage of time, so we may as well use it!
This is important to understand when maximizing the capabilities that a rebreather affords: A PO2 of 1.0 bar allows for five hours of daily diving on CNS tables, and with no pulmonary penalty for multi-day events. I originally designed RD1 for working to this threshold, where the scrubber offers a conservative five hours (based on 1 ATA testing at NOAA rebreather performance criteria) and carries five hours of oxygen based on an assumed metabolic consumption of 1 lpm (368 liters/AL13).
For conservatism, I always plan that oxygen is my limiting consumable so, with the likelihood of getting a somewhat short fill in a 3000 psi cylinder, running down my oxygen over three to five hours was the go/no-go gauge. With attention to my loop flushing technique during pre-dive and monitoring the loop, I was able to enjoy and benefit from countless three-plus hour duration dives on my new RD1 units.
After a few seasons of diving an oxygen-only unit in this fashion, I felt that a level of rebreather proficiency had been attained that would have otherwise been unattainable, and that proficiency has made my mixed-gas diving much easier as well—the perceived complexity has been alleviated.
A Training Opportunity
While up to my elbows in mud for hundreds of hours digging clams, I had nothing but time to think through this perceived complexity issue, and I believe that we’re skipping a step within contemporary training regimens that may be part of the reason why broader market acceptance has not been achieved.
An open question is, “Can we train an open-water diver on a rebreather from Day 1?” Well, yes, but does it need to be (or should it be) a mixed-gas unit which introduces the ‘perceived complexity’ (dynamic gas contents) that often drive people away? I’m proposing to not even go there at all. Eliminate the complexity that comes with mixing gas in the loop altogether and put the new or novice diver on any rebreather, with only oxygen, and introduce rebreather fundamentals.
Current standards and training programs are written for mixed-gas rebreathers from Mod 1 through Mod 3 or similar. Oxygen rebreathers are not presently considered within this paradigm, though it should be borne in mind that disabling the diluent on any mix rebreather effectively creates an oxygen rebreather, which consequently simplifies the overall system and reduces certain risks for training purposes.
I ran an experiment with not-yet-certified, open-water students, introducing them to our RD1 units in a pool. Within minutes, every student took to the system very well. This was an isolated event, though the takeaway was several-fold. First, the students knew enough about breathing off of a second stage that I could emphasize simply ‘when in doubt, bail out.’
Second, with a good observable (by me, the instructor) oxygen flush, we eliminated any concern about hypoxia (an important skill to engrain for future gas dives during the first and last 6 m/20 ft of depth). The exercise was able to focus on just breathing, managing a breathing loop, understanding what to do with some gurgles, basic buoyancy, and bailing out. It was easy, unintimidating, and brought smiles to faces, the way diving should.
Now having worked with numerous new-to-rebreather divers using RD1 and oxygen-only fundamentals through a simplified program that I’ve developed, my observation has been that there is tremendous value starting out in this overlooked gap—arguably “Mod 0,” from which the rest becomes much easier in theory and in practice since the system and methods of rebreather diving in general can be taught, rather than a specific unit being taught (each with nuances related to diluent management). On any rebreather, eliminating the perceived complexity (dynamically diluting the loop) leaves us with an oxygen-only unit to start with the basics.
In very little training time (one to two days), and with only entry-level background know-how, it’s within reach to enable the new, young, enthusiastic diver a five-hour-per-day experience in the shallows. Within this refreshed paradigm, the diver can attain proficiency with loop management and basic maintenance, adopt rebreather theory as part of their baseline knowledge, and have experiences that are only possible with a rebreather. From there, I’ve experienced that students very quickly realize on their own what needs to happen to dive deeper—dilute the breathing gas. The student learns the ‘why’ on their own before the ‘how,’ presenting an organic path to a mix unit.
“We reached out to one training agency who was rather forward, stating, ‘We don’t support oxygen rebreathers,’ which I found confusing — why omit this ultra simplified technique?”
We’ve successfully instituted this ‘Mod 0’ training on the RD1 unit with the University of Arizona’s Scientific Diving Program, where it’s proven to be a valuable tool and technique for research. In an effort to expand the opportunity, we reached out to one training agency who was rather forward, stating, ‘We don’t support oxygen rebreathers,’ which I found confusing — why omit this ultra-simplified technique?

Current Opportunities: Kitting Up!
RD1 units, as conceived, are amazing tools; I and others are using them routinely for a variety of shallow water work. Over the past few years, I’ve organically moved components to a production state with partners—all critical components are produced by ISO9001 manufacturers. For those already expert in the field, we offer a ‘kit’ unit which allows the diver to build out to suit. We have end users staying true to its shallow roots, and also evolving them to mix units.
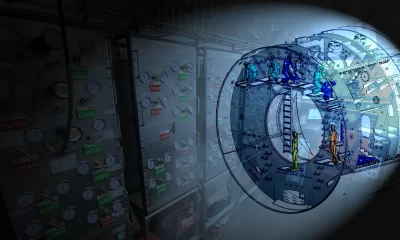
RD1’s inherent simplicity provides an open architecture or building–block-like approach, allowing the end user to reconfigure and evolve the system for their requirements. Conceptually, an RD1 oxygen-only diver could re-plumb to have a very nice mCCR, and then again incorporate any number of accessories for desired features. From the development standpoint, we intend to continue to develop RD1 accessories and upgrade pathways. Just one accessory we’ve been very happy with is our Mouthpiece Retaining Strap (MRS).
“My hope and expectation is that both the oxygen-only fundamentals concept and the RD1 unit itself prove somewhat disruptive.”
My hope and expectation is that both the oxygen-only fundamentals concept and the RD1 unit itself prove somewhat disruptive. As a methodology, simplified training at or near ‘Day 1’ will broaden the end user population which will, in turn, create the need for alternate training paradigms that accommodate specific development paths.
I very much want to see people build off this platform as it becomes recognized that the best rebreather for Rhode Island clams may be different than the one for New Jersey wrecks and Florida caves and Caribbean reefs and elsewhere. However, at its core, a rebreather is a rebreather is a rebreather. We can better institute that mentality if we are instructing oxygen-only fundamentals.
This approach further disrupts current conventions in third party testing. It’s extremely important to understand performance criteria windows, practical limitations of components, and overall system architecture, although the industry is already having to contend with the multitude of aftermarket components being routinely integrated into ‘tested or approved’ units that may negate the initial testing altogether.
A ‘Day 1’ unit and associated knowledge base should eventually take us down a path similar to using a regulator. That level of utility will create the true rebreather market opportunity that would benefit all of us.

To participate in the Rebreather Day 1 discussion, join the Facebook Group: Rebreather Day 1 (RD1)
RD1 Oxygen Rebreather Kit: Kit System (Back Mount)
DIVE DEEPER
InDEPTH: Portable Habitats: New Technical Diving Capabilities are Well Within Reach by Mike Lombardi
InDEPTH: Professor achieves an underwater first – ‘camping’ by Mike Lombardi
InDEPTH: Decompression Habitats Are Ascendent by Andy Pitkin
Inner Space Explorers: The ISE Oxygen Rebreather Program

Michael is a Rhode Island USA based diving contractor, scientist, inventor, and entrepreneur. He has amassed more than 5000 working dives in very challenging conditions – ranging from inshore marine construction to deep mesophotic coral reefs. He has been diving rebreathers since 2003. Michael Co-Chairs the Marine Technology Society’s Diving Committee and is widely published in the field. His company has developed portable habitats, undersea tooling, and custom rebreathers all for use within scientific and industrial projects. More on Lombardi Undersea LLC can be found at www.lombardiundersea.com. Michael’s work in the community can be found at www.oceanopportunity.com. You can reach him at: [email protected]