Education
Gradient Factors in a Post-Deep Stops World
World-recognized decompression physiologist and cave explorer David Doolette explains the new evidence-based findings on “deep stops,” and shares how and why he sets his own gradient factors. His recommendations may give you pause to stop (shallower).
by Associate Professor David J. Doolette
Gradient factors are mechanisms which modify the decompression stops prescribed by the Buhlmann ZH-L16 decompression algorithm. ZH-L16 is a “gas content” algorithm, which tracks the uptake and elimination of inert gas in notional tissue compartments and schedules decompression stops to not exceed specified maximum permissible inert gas partial pressures in the compartments. When such maximum permissible inert gas partial pressures are specified for decompression stop depths, they are referred to as M-values.
Gradient factors (GF) modify M-values (and consequently allowed gas supersaturation) to a fraction of the difference between ambient pressure and the original M-value. Thus, GF 80 modifies the M-value to 80% of the difference between ambient pressure and the original M-value. Typical proprietary implementations of the GF method require the diver to select two gradient factors: GF low modifies the M-values for the deepest decompression stop, and GF high modifies the M-value for surfacing (often designated as GF low/high, e.g. GF 20/80). The algorithm then interpolates a series of modified M-values in between these two user-specified points. If the GF low is set less than 100%, this forces deeper stops to limit supersaturation in the fast tissues early in the ascent, and setting the GF high to less than 100% will produce longer, shallower stops to reduce supersaturation in the slower tissues in the latter phase of the ascent
In contrast to gas content decompression algorithms, bubble decompression algorithms (VPM-B is one such algorithm familiar to GUE divers) characteristically prescribe deeper decompression stops. In simple terms, bubble decompression algorithms favor deeper stops to limit supersaturation and thereby bubble formation early in the decompression, whereas traditional gas content decompression algorithms favor a more rapid ascent to maximize the inspired–tissue gradient of inert gas partial pressures to maximize tissue inert gas washout.
New Findings on Deep Stops
Deep stops came to the attention of early technical divers in the form of empirical “Pyle stops,” a practice serendipitously developed by ichthyologist and technical diving pioneer Richard Pyle, arising from a requirement to vent the swim bladders of fish specimens collected at great depth before arriving at his first decompression stop. There followed a strong trend toward the adoption of bubble algorithms, and also for the use of gradient factors to force gas content algorithms to impose deep stops (for instance, using GF low values of 30% or less). Based largely on supportive anecdotes, a widespread belief emerged among technical divers that deep-stop decompression schedules are more efficient than shallow-stop schedules. Efficiency, in this context, means that a schedule of the same or even shorter duration has a lower risk of DCS than some alternative schedule.
However, since about 2005, evidence has been accumulating from comparative decompression trials that shows deep stops are not more efficient, and possibly less efficient, than shallow stops.
However, since about 2005, evidence has been accumulating from comparative decompression trials that shows deep stops are not more efficient, and possibly less efficient, than shallow stops. Most studies have used venous gas emboli (bubbles) as an indicator of comparative risk of decompression sickness (DCS). Blatteau and colleagues compared dives using French Navy air and trimix decompression tables (relatively shallow stop schedules) to experimental schedules with added deep stops and longer total decompression time (similar to Pyle stops). Despite longer total decompression time, the deep stops schedules resulted in either the same or more VGE than the shallow stops schedules, and some cases of DCS.1

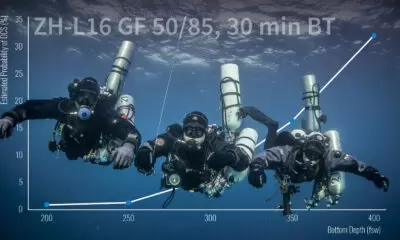
Spisni and colleagues compared trimix dives conducted using a deep stops schedule (ZH-L16 with GF 30/85) to an even deeper stops schedule with longer total decompression time (a UDT version of ratio deco) and found no difference in VGE.2 An as-yet-unpublished study compared trimix dives using a DCAP shallow stops schedule to a ZH-L16 GF 20/80 deep stops schedule with similar total decompression time, and the deep stops schedule resulted in significantly more VGE.3 A large study conducted by the U.S. Navy compared the incidence of DCS in air decompression schedules for 30 minutes bottom time at 170 fsw bottom for a gas content algorithm with the first stop at 40 fsw (shallow stops) or a bubble algorithm with the first stop at 70 fsw (deep stops). The shallow stops schedule resulted in 3 DCS in 192 man-dives and the deep stops schedule resulted in 11 DCS in 198 man-dives.4
What To Do About Gradient Factors
The emerging body of evidence against deep stops suggest common gradient factor setting should be modified to de-emphasize deep stops. Fraedrich validated dive computer algorithms by comparing them to well-tested U.S. Navy decompression schedules, including the schedules from the deep stop study outlined above. For that dive, ZH-L16 with a GF low >55% (e.g. GF 55/70) produced a first decompression stop between 70 and 40 fsw.5 Tyler Coen at Shearwater Research Inc. noted that GF settings recommended by Fraedrich modify ZH-L16 M-values so that approximately the same level supersaturation is allowed at all stop depths. To understand this requires delving a little further into M-values.
The emerging body of evidence against deep stops suggest common gradient factor setting should be modified to de-emphasize deep stops.
M-values are typically a linear function of stop depth. In older algorithms such as ZH-L16, the M-value generating functions have a slope greater than one (in ZH-L16, the slopes are the reciprocals of the “b” parameters), resulting in increasing supersaturation allowed with increasing stop depth. In more modern algorithms developed by the U.S. Navy since the 1980s, including the one used to produce the shallow stops schedule in the study outlined above, the slope of the M-value generating functions are generally equal to one, so that the same level of supersaturation is allowed at all stop depths. This results in modestly deeper stops than older algorithms, but still relatively shallow stops compared to bubble models.
With this information in mind, I set my GF low to roughly counteract the ZH-L16 “b” parameters (I have been using Shearwater dive computers with ZH-L16 GF in conjunction with my tried and true decompression tables for about three years). In ZH-L16, the average of “b” parameters is 0.83. I choose my GF low to be about 83% of the GF high, for instance GF 70/85. Although the algebra is not exact, this roughly counteracts the slope of the “b” values. This approach allows me to believe I have chosen my GF rationally, is not so large a GF low as I am unable to convince my buddies to use it, and satisfies my preference to follow a relatively shallow stops schedule.
This article was prepared by Assoc. Professor Doolette in his personal capacity. The opinions expressed in this article are the author’s own and do not reflect the view of the Department of the Navy or the United States government.
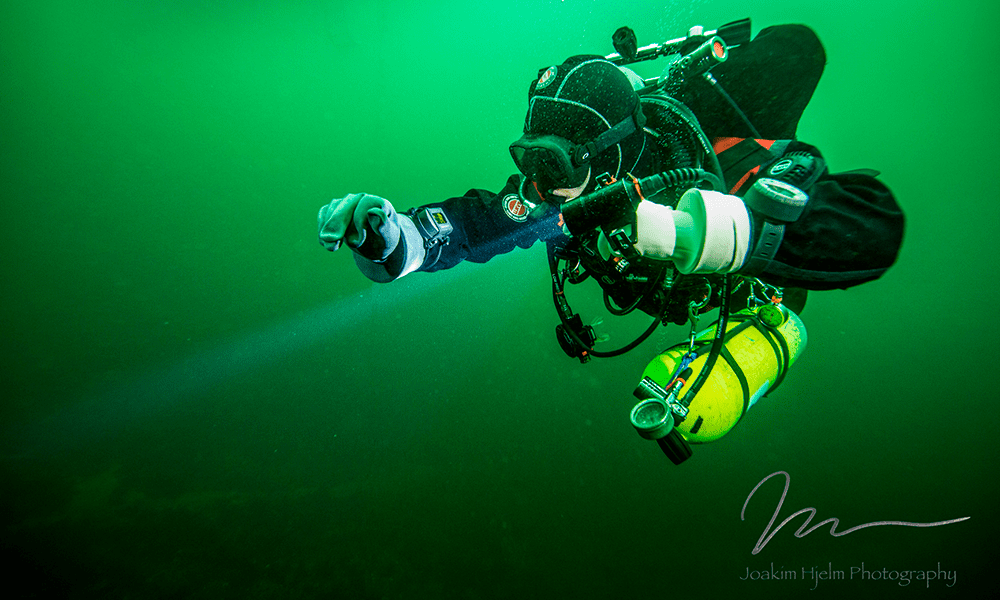
Header image: Joakim Hjelm
1. Blatteau JE, Hugon M, Gardette B. Deeps stops during decompression from 50 to 100 msw didn’t reduce bubble formation in man. In: Bennett PB, Wienke BR, Mitchell SJ, editors. Decompression and the deep stop. Undersea and Hyperbaric Medical Society Workshop; 2008 Jun 24-25; Salt Lake City (UT). Durham (NC): Undersea and Hyperbaric Medical Society; 2009. p. 195-206.
2. Spisni E, Marabotti C, De FL, Valerii MC, Cavazza E, Brambilla S et al. A comparative evaluation of two decompression procedures for technical diving using inflammatory responses: compartmental versus ratio deco. Diving Hyperb Med 2017;47:9-16.
3. Gennser M. Use of bubble detection to develop trimix tables for Swedish mine-clearance divers and evaluating trimix decompressions. Presented at: Ultrasound 2015 – International meeting on ultrasound for diving research; 2015 Aug 25-26; Karlskrona (Sweden).
4. Doolette DJ, Gerth WA, Gault KA. Redistribution of decompression stop time from shallow to deep stops increases incidence of decompression sickness in air decompression dives. Technical Report. Panama City (FL): Navy Experimental Diving Unit; 2011 Jul. 53 p. Report No.: NEDU TR 11-06.
5. Fraedrich D. Validation of algorithms used in commercial off-the-shelf dive computers. Diving Hyperb Med 2018;48:252-8.
Dive Deeper:
InDepth: Variable Gradient Model: An Approach To Create More Efficient Decompressions by Kevin Gurr
PADI recently published an excellent post, “Evolving Thought on Deep Decompression Stops,” by John Adsit, on the subject of Deep Stops.
Alert Diver magazine published a profile and interview with Doolette in the Fall of 2016.
The Math behind the ZH-L16 Model: Bühlmann established, by means of many hyperbaric chamber experiments with volunteers, how much supersaturation the individual tissue compartments can tolerate without injury. He expressed the relationship through the following equation:
pamb. tol. = (pt. i.g. – a) ·b
or
pt. tol. i.g. = (pamb / b) + a
pamb. tol. – the ambient pressure tolerated by the tissue
pt. i.g. – the pressure of the inert gas in the tissue
pt. tol. i.g. – tolerated (excess)pressure of the inert gases in the tissues
pamb – current ambient pressure
a, b – parameters of the model ZH-L16 for each tissue. “a” depends on the measure unit of pressure used, while “b” represents the steepness of the relationship between the ambient pressure pamb. and the pressure of inert gas in the tissue pt. i.g. The first equation shows which lower ambient pressure pamb. tol. will still be tolerated at the actual pressure of inert gas in the tissues pt. i.g. The lower equation shows which level of supersaturation pt. tol. i.g. can be tolerated at a given ambient pressure pamb for a given tissue.
Dr. David Doolette began scuba diving in 1979 and was introduced to the sinkholes and caves of Australia in 1984. Around this time, he alternated between studying for his B.Sc. (Hons.) and working as a dive instructor, when he developed an interest in diving physiology. He planned and conducted some of the first technical dives in Australia in 1993. Since being awarded his Ph.D. in 1995, he has conducted full time research into decompression physiology, first at the University of Adelaide, and since 2005 at the U.S. Navy Experimental Diving Unit in Panama City, Florida.
He has been a member of the Undersea Hyperbaric Medical Society since 1987, received their 2003 Oceaneering International Award, and is a member of their Diving Committee. He has also been a member of the South Pacific Underwater Medicine Society since 1990 and served as the Education Officer for five years. He is a member of the Cave Diving Association of Australia, the Australian Speleological Federation Cave Diving Group, Global Underwater Explorers, and the Woodville Karst Plain Project. He remains an avid underwater cave explorer, both near his home in Florida and abroad.