Diving Safety
High Pressure Problems on Über-Deep Dives: Dealing with HPNS
If you’re diving beyond 150 m/490 ft you’re likely to experience the effects of High Pressure Nervous Syndrome (HPNS). Here InDepth’s science geek Reilly Fogarty discusses the physiology of deep helium diving, explains the mechanisms believed to be behind HPNS, and explores its real world implications with über-deep cave explorers Dr. Richard “Harry” Harris and Nuno Gomes. Included is a list of sub-250 m tech diving fatalities.
By Reilly Fogarty
Header image: Original Photo by Sean Romanowski, effects by the team at GUE HQ
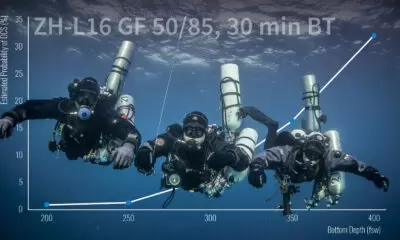
There aren’t many technical divers exploring deeper than 153 m/500 ft on a regular basis—the logistical and physiological demands alone make sure of that. The small group of divers who do reach those depths without saturation chambers or other professional accoutrements face a daunting host of new concerns. At these depths, decompression models aren’t as well validated, and dives require precise gas planning and acknowledgement of extreme environmental exposures.
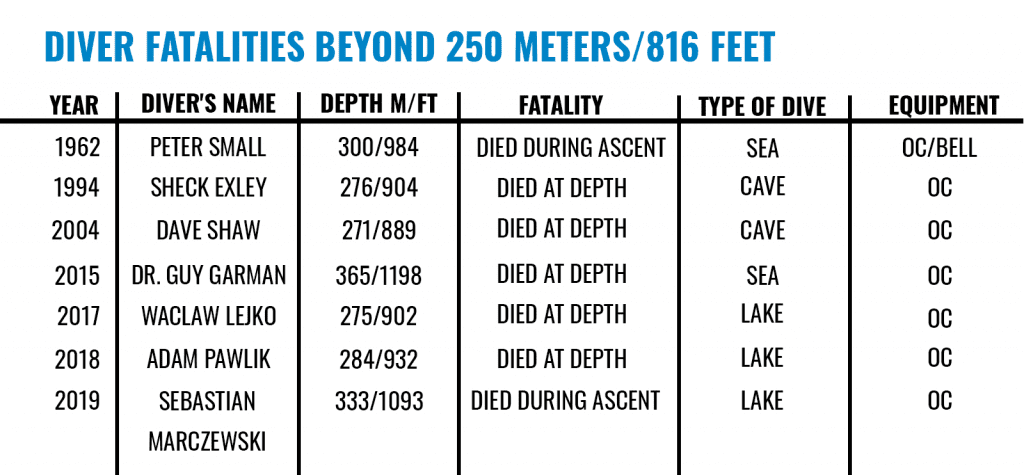
As if decompression illness (DCI) and oxygen toxicity risks weren’t enough, divers must prepare to deal with the possibility that they may get to depth and experience vertigo, confusion, seizures, and a varied list of other neurological maladies—sometimes without warning. These symptoms are the result of high-pressure nervous syndrome (sometimes called high-pressure neurological syndrome) or HPNS. Symptoms of HPNS are highly variable but primarily affect those who descend rapidly to 153 m/500 ft or deeper. HPNS may have played a role in the death of legendary cave explorer Sheck Exley, and it may have caused numerous close-calls in deep cave and wreck explorations. But, the extreme depth required to experience onset has relegated research and education on HPNS to a niche corner of the diving community—one with significant interplay with the commercial saturation diving world and the most extreme sport communities.
The Physiology of Deep Helium Diving
In 1961, G.L. Zal’tsman, who headed the Laboratory of Hyperbaric Physiology, St. Petersburg, Russia, first identified what would eventually become known as high-pressure nervous syndrome. The political climate of the period limited access to his work in the west, so credit for the discovery is often shared with Peter Bennett, D.Sc, who published a paper on the subject in 1965. While politics and international tensions separated them, both researchers described what they called “helium tremors” that occurred during experiments with military subjects. Using gases with the high helium content required to manage narcosis at depth, participants in these studies were observed experiencing uncontrollable muscle tremors upon compression in a chamber.
At the time, it was unknown if this was a function of the helium in their breathing gas or an effect of depth. The term “high-pressure nervous syndrome” originated just a few years after Zal’tsman’s study, when R.W. Brauer identified changes in the conscious states and electroencephalography data from subjects in a chamber dive to nearly 368 m/1,200 ft. In the decades since, several studies further illuminated what we now know as HPNS, primarily as a result of research into deep sea exploration from the 1970s to early 1990s. As it stands now, HPNS is primarily identified by a decreased mental status, dizziness, visual disturbances, nausea, drowsiness, muscle tremors, and seizures in divers rapidly reaching depths of 153 m/500 ft or more, or exploring the extremes of depth closer to 306 m/1,000 ft at any rate of compression while breathing a high helium content gas.
The prevailing theory is that a combination of speed of compression during descent, and the absolute pressure at depth, cause these symptoms. Symptoms are rare during dives above 153 m/500 ft, but dives that exceed that depth, or that reach depth quickly, increase the likelihood of symptom evolution. Symptoms do not appear to correlate to each other, and individual susceptibility is highly variable, which makes predicting onset difficult. Some researchers also theorize that there are two separate conditions caused individually by compression (the symptoms of which diminish at depth) and total pressure (the symptoms of which persist throughout the bottom portion of a dive). This two-part explanation for HPNS symptoms provides some interesting avenues for future research and could help solidify some of the theorized mechanisms underlying the condition, but it has yet to be expanded upon in a significant way.
The mechanism behind HPNS has yet to be proven, but most researchers choose to work upon the basis of a few reasonable theories. The first relies on the compression of the cell membranes in the central nervous system. In this model, the rapid compression of the lipid components of these membranes may alter the function of the inter-lipid structures that facilitate signal transmission within the central nervous system. This change in structure could facilitate hyperexcitability of some nervous system pathways and cause the types of tremors and seizures associated with serious HPNS cases. This membrane compression could also alter the signaling pathways required for motor function and cognition, resulting in confusion and assorted neurological symptoms that sometimes occur in divers with HPNS.
Another model focuses on the role of neurotransmitters themselves, rather than their signaling receptors. The various iterations of this model examine the effects of pressure and varying helium/oxygen exposures on the production or reception of these transmitters. In some ways, this method resembles our understanding of oxygen toxicity mechanisms, which could lead to some interesting interplay between future research projects and the balancing of oxygen and helium exposures at extreme depth. Some of the more promising studies in this area show evidence of NMDA receptor antagonists reducing convulsions in animal models, and describe the effectiveness of increased dopamine release in preventing increased motor activity under extreme pressure in rat models.
A third model focuses on the effect of helium on HPNS risk. This model functions on a yet-unidentified mechanism, but explores the potential distortion of lipid membranes by helium at depth. The data from these studies suggests that high pressure helium—not high hydrostatic pressure—may alter the tertiary structure of protein-lipid interactions and change signaling pathways within the nervous system. Numerous other avenues for research exist in this niche, including projects working on a great number of neurotransmitter related conditions and pre-treatment protocols for HPNS, oxygen toxicity, and possibly related normobaric diseases. Any of these models could prove accurate, but the interplay between the many neurotransmitters makes it most likely that a combination of these models will best illustrate what occurs in-situ.
Real-World Experiences
Experienced firsthand, HPNS is far less academic, but equal parts confounding and terrifying. The variable onset and sometimes ambiguous symptom presentation make it difficult to discern from other conditions, and mild symptoms can be easily written off. By the same token, however, a serious bout of tremors or confusion as a result of a rapid descent to deep water can leave a diver terrified and unable to act. Dr. Richard “Harry” Harris, SC OAM, is a physician and technical diver with years of exploration in deep caves and shipwrecks. His experiences with HPNS mirror that of many. Most often, he’s observed symptoms like trembling hands or loss of coordination that could be attributed to either HPNS or the adrenaline rush of a fast hot-drop from a boat in heavy seas.

On one recent dive to 150 m/490 ft, Harris described becoming temporarily incapacitated on the bottom due to minor tremors, finding himself unable to clip his strobe to the shot line. The symptoms resemble common descriptions of mild HPNS symptoms, but the relatively shallow (in terms of HPNS, at least) depth still gives him pause when he tries to discern the specific cause of the symptoms. Dives past 200 m/656 ft have provided similar conundrums, but Harris has experienced tremors at extreme depths with enough regularity to notice that he is somewhat more susceptible than his regular dive buddy Craig Challen. “This [variation in symptom onset and presentation] has really made me question again the role of the mental state, approach, and perhaps even intentional mindfulness on these symptoms,” explains Harris.

By focusing on gas choices that strike a balance between gas density and the high concentrations of helium that can cause HPNS symptoms, and by descending relatively slowly, Harris has managed to alleviate symptoms on much deeper dives. A recent 245 m/799 ft dive with an intentionally slowed descent gave him none of the same complaints as his rapid descents to shallower water and felt “like a [much shallower] 150 m/490 ft dive.”

It’s worth noting at this point that Harris and Challen are extraordinarily capable and experienced divers, and HPNS is a condition that shouldn’t be taken lightly. Their approach—a combination of conservatism and safety—is likely key to their management of HPNS on extremely deep dives. Other divers, some equally experienced, have not been as fortunate in the past.
Sheck Exley reported a particularly bad case during a dive to 210 m/689 ft, with vision blurred to the extent that he was “looking through small circles with black dots, and started convulsing.” Despite these symptoms, he continued his dive, and proceeded to a maximum depth of 263 m/863 ft. It’s thought that Exley’s eventual death during an attempt to descend past 305 m/1,000 feet in the Mexican Zacatón cave system could have been caused in part by HPNS symptoms exacerbated by narcosis.

Nuno Gomes, a technical diver who holds several Guinness World Records for depth in open water and in caves, has also become intimately acquainted with HPNS, experiencing the following during a world record dive:
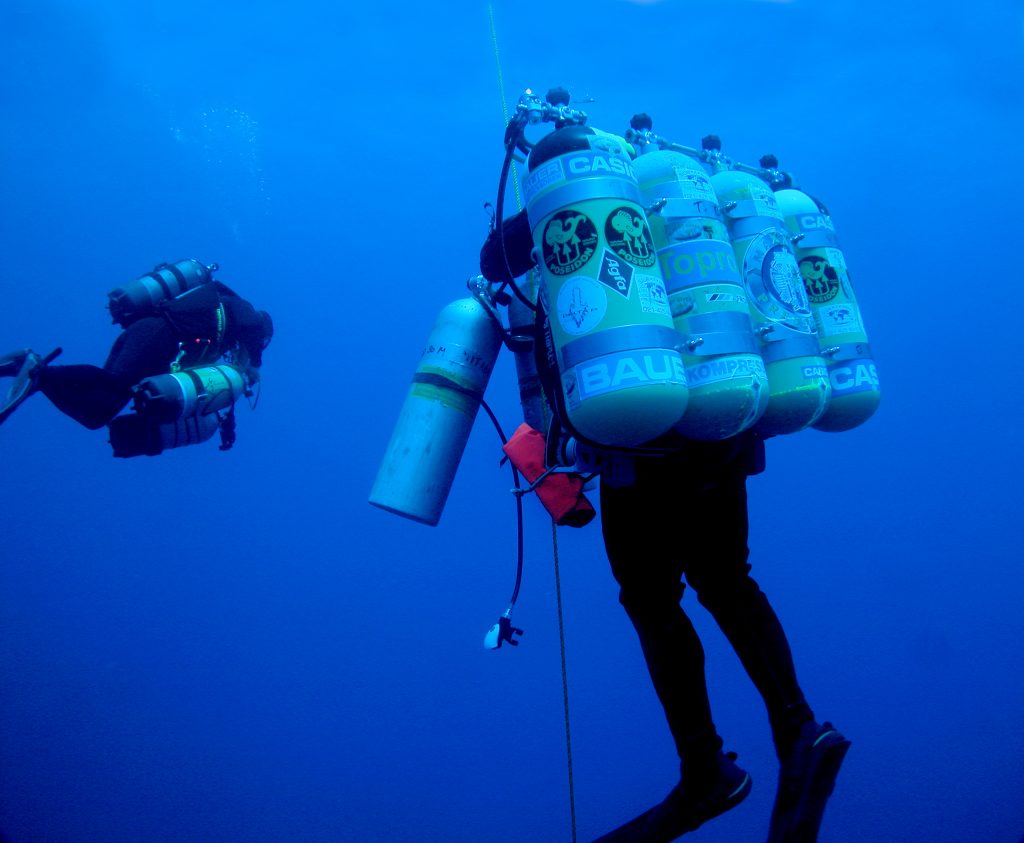
“As I descended past 250 m/816 ft, the HPNS set in. At first, relatively mild, then fairly strong. And later on, the symptoms became so extreme that my whole body shook uncontrollably. One other problem was lack of coordination of movement. I felt severely narcosed on my bottom trimix of 3.15/85. It had only a calculated END of 40 m/131 ft. From my experience, a more realistic narcosis level was 78 m/256 ft as calculated using the Total Narcotic Depth (TND). When I reached the tag marked 315 m/1,033 ft at an actual depth of between 322 m/1,056 ft and 323 m/1061 ft, I realized that this was as far as I was able to go. I was not sure that I would be able to return if I went any deeper. At that stage, I was not sure that I would be able to swim up from that depth.”
Gomes’s regular attempts to reach extreme depth made him uniquely prepared to identify symptoms of HPNS as they appeared, but even with his breadth of experience, the effects of the condition could have become lethal if allowed to continue.

Statistically, there just aren’t enough documented cases of HPNS to make for a meaningful analysis, but these incidents can provide a basis for education. The symptom severity and onset variability is enormous, but there are some trends that can be pulled from the stories of Harris, Exley, and Gomes. How to integrate those in your dive plan without meaningful data to back them up, however, falls to personal choice.
Planning for the Future
There are more than a few good reasons not to end this piece with a “how-to” on diving past 153 m/500 ft. With regard to HPNS specifically, the reality is that we just don’t know enough about the mechanisms that cause the symptoms divers experience. What we have is an understanding that high helium content and rapid descents likely contribute to HPNS risk, some people are more susceptible than others, and the symptom presentation is not uniform or predictable. Beyond these fundamental constants, we must piece together what we know from the limited research we do have and the experiences of others.
The data on compression speed appears to be pretty clear: HPNS symptoms may not be entirely preventable, but the risks can be somewhat ameliorated by slowing our descent speeds. There also appears to be an opposing effect between helium and nitrogen content in our breathing gas. This is likely due to changes in the structures of the membranes surrounding our central nervous system caused by helium and other inert gases, requiring divers to balance potential narcotic effects and HPNS risk in gas planning.
Using nitrogen as a protective gas seems counterintuitive, but in some extremely deep dives, adding just 5% nitrogen to a heliox mixture appeared to dramatically reduce HPNS symptoms in divers. However, the extent of practical efficacy remains to be seen. Promising studies researched using hydrogen to minimize HPNS risk, but this avenue of research is prohibitively expensive and logistically challenging due to the inherent fire risk.
The onset of HPNS symptoms also appears to be relatively gradual, although it’s important to recognize that not all data supports this and rapid onset can occur. With slow descent rates and intelligent gas choices, it seems unlikely that divers would experience HPNS severe enough to incapacitate them before they had a chance to turn their dive, but that is not to say that it cannot happen or should be ignored as a real concern. Symptoms of HPNS still haven’t been found to correlate with each other, and not only can new symptoms arise quickly, but also the nature of the ailments means that a diver may not be able to identify symptoms until it is too late to react.
The past decade has failed to provide much in significant data on HPNS as it pertains to recreational divers, certainly almost nothing in comparison to the deep-diving heyday that brought about the COMEX tables and Atlantis projects. Going forward, it seems likely that HPNS will become a greater concern. Technical divers will continue to explore the limits of depth with the widespread adoption of rebreathers, persisting in their search for deeper caves and unexplored wrecks. Hopefully, this ongoing—perhaps even increasing—activity will spur more research into HPNS and the potential interplay between the mechanisms of narcosis and oxygen toxicity. Until then, we’ll have to continue to glean what we can from the data we have and the experiences of the more ambitious among us.
References:
- Naquet, R., Lemaire, C., J.-C. Rostain, & Angel, A. (1984). High Pressure Nervous Syndrome: Psychometric and Clinico- Electrophysiological Correlations [and Discussion]. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences, 304(1118), 95-102. Retrieved May 21, 2021, from http://www.jstor.org/stable/2396156
- Talpalar, Adolfo. (2007). High pressure neurological syndrome. Revista de neurologia. 45. 631-636.
- Understanding Oxygen Toxicity: Part 1 – Looking Back
- Pearce PC, Halsey MJ, MacLean CJ, Ward EM, Webster MT, Luff NP, Pearson J, Charlett A, Meldrum BS. The effects of the competitive NMDA receptor antagonist CPP on the high pressure neurological syndrome in a primate model. Neuropharmacology. 1991 Jul;30(7):787-96. doi: 10.1016/0028-3908(91)90187-g. PMID: 1833661.
- Kriem B, Abraini JH, Rostain JC. Role of 5-HT1b receptor in the pressure-induced behavioral and neurochemical disorders in rats. Pharmacol Biochem Behav. 1996 Feb;53(2):257-64. doi: 10.1016/0091-3057(95)00209-x. PMID: 8808129.
- Bliznyuk, A., Grossman, Y. & Moskovitz, Y. The effect of high pressure on the NMDA receptor: molecular dynamics simulations. Sci Rep 9, 10814 (2019). https://doi.org/10.1038/s41598-019-47102-x
- High Pressure Neurological Syndrome, DIVER (2012) by Dr. David Sawatzky
Dive Deeper:
InDepth: Diving Beyond 250 Meters: The Deepest Cave Dives Today Compared to the Nineties by Michael Menduno & Nuno Gomes
World Record Cave Dive – 282.6 m (927 feet) – Nuno Gomes
Pearse Resurgence 2020-Richard Harris and Craig Challen
Diver Records Doom | Last Moments-Dave Shaw
aquaCORPS:Accident Analysis Report from aquaCORPS #9 Wreckers (JAN95):What happened to Sheck Exley? by Bill Hamilton, Ann Kristovich And Jim Bowden
InDepth: Thoughts on Diving To Great Depths by Jim Bowden
InDepth: Playing with Fire: Hydrogen as a Diving Gas By Reilly Fogarty

Reilly Fogarty is an expert in diving safety, hyperbaric research, and risk management. Recent work has included research at the Duke Center for Hyperbaric Medicine and Environmental Physiology, risk management program creation at Divers Alert Network, and emergency simulation training for Harvard Medical School. A USCG licensed captain, he can most often be found running technical charters and teaching rebreather diving in Gloucester, Massachusetts.