DCS
Hyperbaric Chambers Are Turning Away Divers. Will There Be One Nearby When You Need It?
Unfortunately, it’s hard to make a business case for treating divers versus wound and burn care victims. As a result, many hyperbaric chambers in the US no longer treat divers, leaving fewer facilities available for divers in need and increasing their post-dive time to treatment. InDEPTH editor Ashley Stewart reports on this growing crisis in the US and what can be done!
By Ashley Stewart
Steven Wells was diving on the scuttled wreck of the USS Oriskany off the coast of Florida in 2016 when a problem with his buoyancy compensator caused a rapid ascent to the surface.
Wells’ dive buddies followed the emergency action plan for the Oriskany listed on the Florida Fish and Wildlife Conservation Commission’s website at the time and brought Wells straight to Naval Air Station Pensacola, the nearest facility with a hyperbaric chamber. The facility turned him away because there was no one there to run it.
Wells was taken 30 minutes away to Baptist Hospital, which also has a chamber capable of treating his injuries, but the hospital had years earlier decided only to use it for wound care. Doctors there decided Wells would be taken by ambulance more than an hour away to Mobile, Alabama, the nearest facility that accepts divers.
By the time Wells arrived at the only chamber that would help him, it was too late.
“I got a call from the hospital saying, ‘Your husband is on life support. You need to get here now,’” Rachel Wells said of her late-husband of more than 23 years.
Julio Garcia — the program director of Springhill Medical Center’s wound care and hyperbaric facility where Steven Wells was to be treated — told InDEPTH that while no one can be certain how sooner treatment would have affected the outcome of Wells’ case, it would have given him the best chance for a full recovery.
Each year in the US, there are about 400 serious cases of decompression illness (DCI) — a category including both arterial gas embolism and decompression sickness — in divers, according to one 2020 paper. The Divers Alert Network (DAN) hotline dealt with 587 cases annually over the past five years.
The availability of hyperbaric chambers to treat decompression illness is something many divers take for granted. We try to avoid dive-related injuries through training, but expect treatment to be available when we need it.
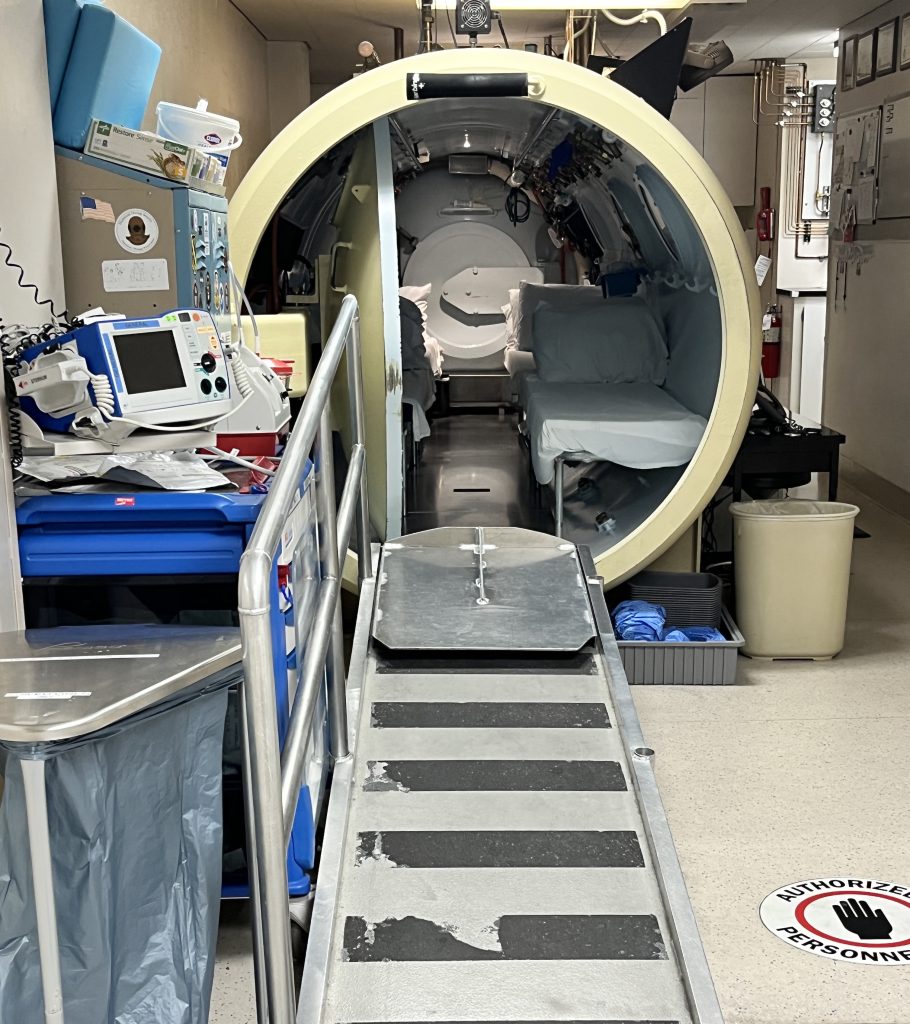
The reality — as Steven and Rachel Wells tragically learned — is that only a minority of divers are close to care for diving-related injuries, according to medical professionals in the field. The estimates vary, but it’s generally believed there are about 1,500 hyperbaric medicine facilities in the US and only 67 are currently treating diving accidents, according to DAN.
The estimates vary, but it’s generally believed there are about 1,500 hyperbaric medicine facilities in the US and only 67 are currently treating diving accidents, according to DAN.
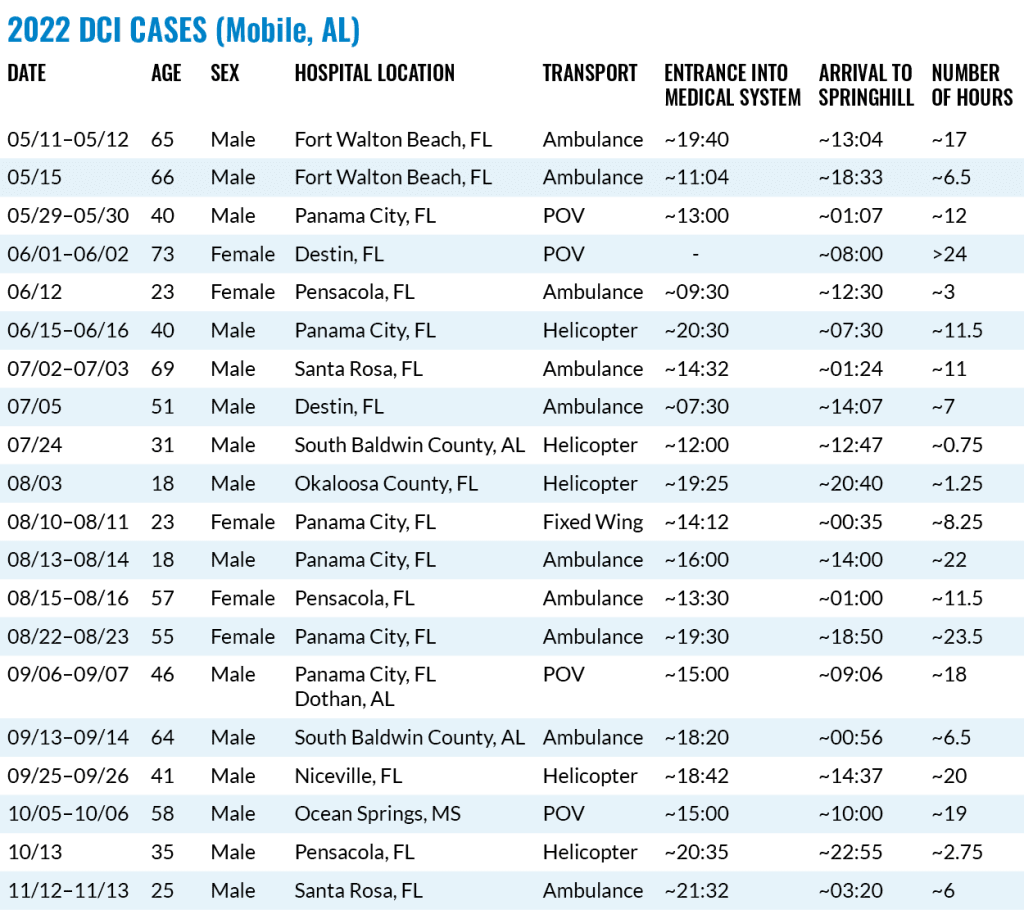
“The problem is only getting worse, not better,” Garcia, the Springhill Medical Center program director, said. Garcia has been sounding the alarm about this problem for more than a decade. His hospital takes patients from as far away as Florida cave country and treated 20 DCI cases in 2022. Those patients had an average transportation time of 11.5 hours, according to an InDEPTH analysis of Garcia’s records.
Florida stands out because it’s a popular diving destination, DAN Research Director Frauke Tillmans said, but the situation is not much better across the US. Many of the 1,500 hyperbaric medicine facilities, like Pensacola’s Baptist Hospital, have transitioned to treating wound care only for economic reasons. Emergency hyperbaric services are expensive to train and staff, and come with increased liability.

Time to treatment can be important in DCI cases
Time is of the essence when treating DCI. Divers Alert Network Director of Medical Services Camilo Saraiva told InDEPTH time to treatment is a “pivotal determinant” when it comes to outcomes for DCI patients. “Swift intervention significantly influences the effectiveness of therapeutic recompression,” Saraiva said.
Decompression sickness, for example, results from rapid changes in pressure and can form gas bubbles in body tissues. Initiating recompression therapy minimizes bubble size and number, Saraiva said, enhancing their elimination and reducing the risk of further vascular obstruction and tissue damage.
“The timely provision of hyperbaric oxygen therapy not only aids in bubble resolution but also mitigates the potential for neurological deficits and other severe complications, highlighting the critical role of early treatment in optimizing outcomes for DCI patients,” Saraiva said.
The 2018 paper “In water-recompression” stated delays to recompression in military and experimental diving are typically less than two hours and more than 90% of cases are completely resolved during the first treatment.
Frank K. Butler and Richard E. Moon, hyperbaric medicine experts, wrote in a 2020 letter to the Undersea and Hyperbaric Medicine journal editors suggesting a minority of patients who need life-saving hyperbaric oxygen treatment (HBO2) are close to a major hospital with a 24-hour emergency hyperbaric facility.
“Despite the urgent need for treatment, most hyperbaric chambers will decline to accept emergent patients at present,” Butler and Moon wrote. “Patients may eventually receive HBO2 but after a significant delay and a transfer of several hundred miles. Many never receive indicated HBO2, often resulting in poorer patient outcomes.”
Patients who are delayed treatment, they wrote, face the possibility in some cases of “death, permanent neurological damage, permanent loss of vision, or loss of an extremity, most of which would have been readily preventable had emergent HBO2 been administered.”
Why fewer chambers treat dive injuries
As recently as two decades ago, according to Butler and Moon, the majority of hyperbaric treatment facilities were available 24/7 to treat emergency patients. The percentage of those facilities now treating emergency patients is unclear, but it’s universally agreed the number has fallen significantly.
The reasons for the loss of emergency HBO2 facilities, Butler and Moon suggest, include “a better economic return when chambers focus on wound care patients as opposed to emergencies; the greater legal liability involved with treating high-acuity emergency patients; and the increased training and staffing requirements that would be required to manage critically ill patients — especially diving injuries and iatrogenic gas embolism patients.”
A letter from an administrator at Baptist Hospital — which sent Steve Wells to Springhill Medical Center — viewed by InDEPTH shows the hospital discontinued hyperbaric emergency services in December 2010, citing lack of staffing for specialty trained hyperbaric physicians who can provide 24-hour patient care. Baptist has yet to respond to InDEPTH’s request for comment.

There’s also the issue of pay. Garcia, the Springhill program director, said the current rate of pay for doctors who administer hyperbaric treatments regardless of length is around $150. A typical hyperbaric treatment for other conditions is about two hours. Diving treatments are usually six or seven, he said. “What doctor wants to get paid $150 to be up all night for seven hours, at that point making less than the technician?” Garcia said. “The fix is that healthcare payers need to pay more for the supervision of the treatment for diving injuries. Make it something that’s worth a doctor’s time besides the goodness of their hearts.”
Silence from lawmakers
Medical and diving organizations in 2020 sent a letter to the House and Senate, federal government agencies, governors of Florida and California, and the American Hospital Association expressing concerns about the lack of availability of chambers to treat diving injuries.
“There are approximately three million recreational scuba divers in the US,” the letter stated. “In the unlikely event that they suffer a diving-related injury, they trust that the US medical system will provide state-of-the-art care for their injuries, but the steadily- decreasing number of hyperbaric treatment facilities in the US willing to treat them emergently for decompression sickness or arterial gas embolism often places them at much greater risk than they realize.”
Garcia has on his own contacted lawmakers, reporters, medical systems — even private space companies like SpaceX because his facility is also the only one nearby treating altitude decompression sickness from space and air travel.
Little has changed, Garcia said.
Garcia showed InDEPTH a 2014 letter from a Defense Health Agency director who said, while there are three Undersea and Hyperbaric Medicine Society-accredited clinic hyperbaric medicine facilities and two additional facilities that can treat civilian emergencies, they are not staffed 24/7 and not designed for patients with other medical illnesses. Garcia at the time requested the creation of a federal grant to support the expansion of 24/7 hyperbaric services, but the director said that was outside of the agencies’ purview.

Two years after this exchange, Steven Wells was taken to and turned away from one of these facilities — the NAS Pensacola, listed on the Florida Fish and Wildlife Conservation Commission’s (FWC) emergency action plan at the time.
The Florida Fish and Wildlife Conservation Commission website now shows a map of the nearly 4,000 artificial reefs across Florida’s 1,350 miles of coastline. Two chambers, one in Mobile, Alabama, and one is Orlando, cover 500 of those miles densely packed with dive locations, according to Garcia.
The FWC website now shows a map of the nearly 4,000 artificial reefs across Florida’s 1,350 miles of coastline. Two chambers, one in Mobile, Alabama, and one is Orlando, cover 500 of those miles densely packed with dive locations, according to Garcia. A report from the University of West Florida estimated the sinking of the Oriskany, scuttled in 2006, generated nearly $4 million for Pensacola and Escambia County in the next year alone.
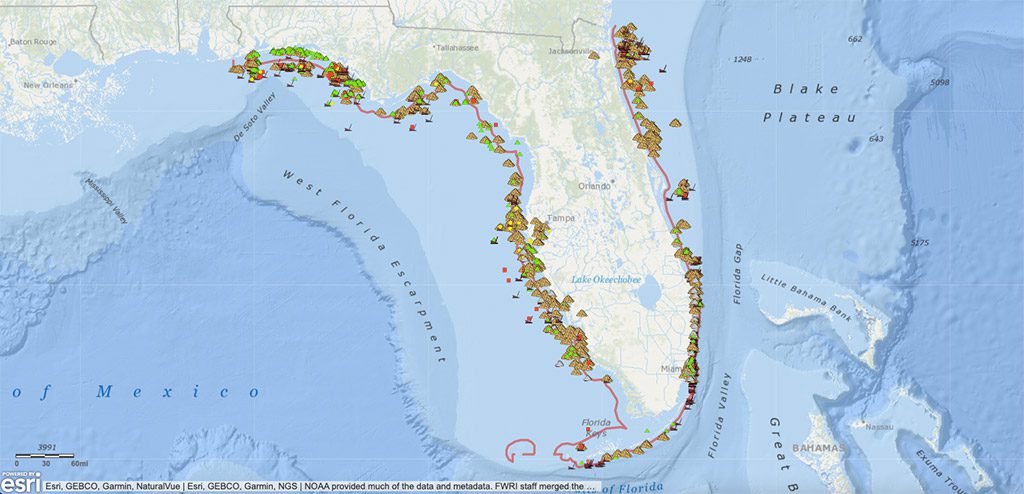
An FWC spokesperson said the agency provides diver safety reminders and recommended actions on its website “as a courtesy” and is not intended for emergency response. FWC and Visit Florida did not respond to inquiries about how much Florida’s government spends on advertising the artificial reefs and other diving activities, or whether any effort to expand the availability of hyperbaric facilities to treat the divers who show up as a result.
“My question is what is my husband’s life worth compared to your chambers,” Rachel Wells, Steven Wells’ widow said. “Why did he have to die?”
DIVE DEEPER
DIVER: A Crisis in Emergency Chamber Availability by Dan Orr (April 2022)
Divenewswire: A Crisis Lurking Below the Surface Emergency Hyperbaric Treatment Availability by Dan Orr (August 2021)
Undersea and Hyperbaric Medicine (2020): Emergency hyperbaric oxygen therapy: A service in need of resuscitation – an open letter by Frank K. Butler, MD, and Richard E. Moon, MD
White paper: Access to emergent hyperbaric oxygen (HBO2) therapy: an urgent problem in health care delivery in the United States (2020)
InDEPTH: A New Look at In-Water Recompression (IWR) (2019) by Reilly Fogarty
Diving and Hyperbaric medicine (2018): In-water Recompression, Doolette DJ and Mitchell SJ
aquaCORPS (1993): In-Water recompression As An Emergency Field Treatment for Decompression Illness by Richard L. Pyle and David A. Youngblood

InDepth Managing Editor Ashley Stewart is a Seattle-based journalist and tech diver. Ashley started diving with Global Underwater Explorers and writing for InDepth in 2021. She is a GUE Tech 2 and CCR1 diver and on her way to becoming an instructor. In her day job, Ashley is an investigative journalist reporting on technology companies. She can be reached at: [email protected].