Latest Features
Rebreather Forum 4 Yields CCR Market Data and Consensus Statements
By Ashley Stewart and Michael Menduno. Images by Jason Brown, BARDOPhotograhic unless noted. Header image: Professor Timmy Gambin discussing their shipwreck documentation efforts.
The latest Rebreather Forum produced the most comprehensive data analysis of the rebreather market to date, and a series of consensus statements to improve safety in closed-circuit rebreather (CCR) diving.
The three-day meeting from 20-22 April in Malta gathered 294 rebreather diving experts to advance and consolidate the diving community’s knowledge of rebreather technology and its use by technical, government and scientific divers, with the goal of improving rebreather diving safety and performance.

What is the Rebreather Forum?
The forum is an industry workshop and scientific meeting with a focus on improving CCR safety. Unlike dive trade shows or conferences, the purpose of the Rebreather Forum is to advance research and develop industry consensus on important topics.
Rebreather Forum is similar to dive-industry workshops like the 1992 Enriched Air Nitrox workshop that gathered diving experts to determine guidelines related to nitrox use, or the Flying-After-Diving workshops in 1989 and 2002 which came up with guidelines for surface intervals in between flying and diving.

RF4 Consensus Statements
The forum produced 28 consensus statements intended to reflect widely supported opinions of RF4 participants. The statements include thematic areas designated “safety,” “research,” “operational issues,” “education and training,” and “engineering.” Authors Simon J. Mitchell and Neal W. Pollock published the statements in full on InDEPTH.
Such consensus statements drive change in the industry. Rebreather Forum 3 attendees, for example, reached a consensus regarding pre-dive checklists, specifically recommending “rebreather manufacturers produce carefully designed checklists” and “training agencies and their instructors embrace the crucial leadership role in fostering a safety culture in which the use of checklists by rebreather divers becomes second nature.”
Since then, pre-dive checklists have been widely adopted. In a pre-RF4 survey, 73% of attendees indicated they “always” use checklists. (There’s still progress to be made. RF4 included a checklist-related consensus statement to strongly advocate for specific critical safety items.)

Rebreather Divers Are Dying At A Rate Of Two to Four Deaths per 100,000 Dives
In addition to consensus statements, RF4 produced the most comprehensive data analysis of the rebreather market to date, thanks to research from Dr. Frauke Tillmans and her team who compiled the data that shows the industry needs to do more to improve safety. “Analysis of contemporary rebreather accident data indicates a continued need for integrated effort to reduce the rates of injury, morbidity, and mortality associated with rebreather diving,” as one consent statement reads.
Tillmans, Divers Alert Network (DAN) research director, revealed insights from an analysis of data from DAN, public surveys, and information supplied by CCR manufacturers to give attendees the best look yet at market, demographic and safety data. Frauke’s research is further explored in this InDEPTH article.
Tillmans estimates that rebreather divers are dying at a rate of 2-4 deaths/100,000 dives, which is not substantially different from the analysis made by Dr. Andrew Fock at RF3.
Tillmans reported that at least 241 rebreather divers have died since RF3 (2012). She estimates that rebreather divers are dying at a rate of 2-4 deaths /100,000 dives, which is not substantially different from the analysis made by Dr. Andrew Fock at RF3. Fock estimated that the risk of dying on a rebreather was 5-10X the risk of open-circuit scuba. (Fock AW Analysis of recreational closed-circuit rebreather deaths. 1998-2010. Diving Hyperb Med 2013 Jun;43(2):78-85). Note by comparison, skydiving deaths ranged from 0.28-0.45 deaths per 100,000 jumps for the period 2018-2021 according to the United States Parachute Association (USPA), making rebreather diving 10x as risky as skydiving.
By comparison, skydiving deaths ranged from 0.28-0.45 deaths per 100,000 jumps for the period 2018-2021, making rebreather diving 10x as risky as skydiving.
Using data from the DAN hotline, RF4 participants, and a related survey, Tillmans estimated the mean age of CCR divers is 42-46 years, the CCR diving population is between 84% and 95% male, and certified for an average of six years.
In addition to summarizing the number of reported fatalities, Tillmans calculated the approximate installed base of sport rebreathers in the field, based on information from 20 of 24 sport CCR manufacturers. She estimates between 25,000 to 35,000 rebreather units are on the market today. According to our Pre-RF4 survey, rebreather divers own 1.7 eCCRs on average, so we might estimate that there are 15,000-20,000 rebreather divers up from a very rough estimate of 10,000-15,000 from RF3.
In parallel to Tillman’s data gathering in an effort spearheaded by Brian Carney, president, TDI, a group of training agencies agreed to submit their CCR training data from RF3 (2012) to 2022, to DEMA’s market research firm DP Research Solutions to consolidate and anonymize the agencies’ rebreather training data.
The analysis from DP Research found agency rebreather certifications issued annually ranged from about 3,500 to 5,200 per year between 2012 and 2022, with 2022 being the strongest year for certifications. The data includes certifications from entry-level to advanced, submitted by training agencies BSAC, GUE, SDI/TDI, FFESSM, SSI, PADI, IANTD, and Dive RAID.
More data is needed to understand and make improvements to rebreather safety. For this reason, one product of RF4 was a consensus statement advocating “self-reporting of diving mishaps and near-misses, and reporting of fatalities, to the DAN diving incident reporting system.”
RF4 Overview
RF4 included 22 presentations from experts including Dr. Richard “Harry” Harris, who this year completed the first reported CCR dive with hydrogen as a diluent, and prominent dive-science researchers.
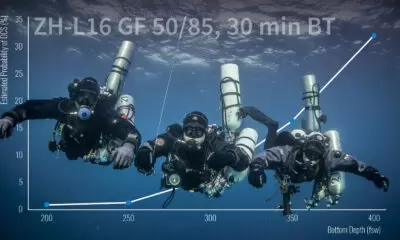
David Doolette of the U.S. Navy Experimental Diving Unit, for example, presented on advances in decompression theory and practice, including the role of biomonitoring for venous gas emboli and heart rate variability in decompression planning. Pollock gave a presentation on hazards of CCR diving and Mitchell gave a presentation about developments in carbon dioxide monitoring, calling for the development of so-called end-tidal CO2 monitoring to detect levels in the diver. Full videos of the presentations will be available later this year.

The meeting gathered 294 attendees including CCR manufacturers, dive science researchers, and training agencies including: 83 vendor representatives, 9 external press representatives, 29 exhibitors, 17 sponsors, and five media partners. There were 111 try-dives held at a local pool in the days leading up to the conference. Units included the Liberty back-mount and side-mount units, Lungfish S. Loop and Alliance, Fathom MK III, XCCR, rEvo / Horizon, and Triton.
The latest forum, Rebreather Forum 4, is the fifth such trade and scientific meeting held by the diving community. The original Rebreather Forum was held in May 1994, in Key West, Florida, followed by RF2 in September 1996 in Redondo Beach, California, and RF3 in May 2012 in Orlando, Florida. A related event, Rebreathers and Scientific Diving, was held in February 2015 on Catalina Island, California.
Because the forum is held only when there is a need, it does not follow a specific schedule like an annual conference might. Rebreather Forum 5 is expected in the late 2020s.
RF4 would like to thank all of its sponsors and exhibitors, and our volunteers! Thank you!

DIVE DEEPER
Scubanomics: Expectations For Rebreather Forum 4 & A Glimpse Into The State of Rebreather Diving. The survey was conducted in March & April of 2023 among Rebreather Forum 4 attendees, presenters, exhibitors & sponsors.
DAN Europe blog: Highlights from the first day of Rebreather Forum 4 by Tim Blomëke
DAN Europe blog: What You Missed from Day Two of Rebreather Forum 4 by Tim Blomëke
DAN Europe blog: Insights and Breakthroughs: A Recap of Day Three at Rebreather Forum 4 by Tim Blomëke

InDepth Managing Editor Ashley Stewart is a Seattle-based journalist and tech diver. Ashley started diving with Global Underwater Explorers and writing for InDepth in 2021. She is a GUE Tech 2 and CCR1 diver and on her way to becoming an instructor. In her day job, Ashley is an investigative journalist reporting on technology companies. She can be reached at: [email protected]

Michael Menduno/M2 is InDepth’s editor-in-chief and an award-winning journalist and technologist who has written about diving and diving technology for more than 30 years. He coined the term “technical diving.” His magazine “aquaCORPS: The Journal for Technical Diving” (1990-1996) helped usher tech diving into mainstream sports diving, and he produced the first tek.Conferences and Rebreather Forums 1, 2 and 4. In addition to InDepth, Menduno serves as an editor/reporter for DAN Europe’s Alert Diver magazine, a contributing editor for X-Ray mag, and writes for DeeperBlue.com. He is on the board of the Historical Diving Society (USA), and a member of the Rebreather Training Council.