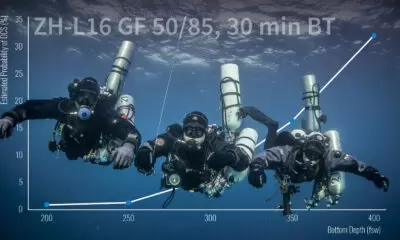
DCS
Rules of Thumb 2: Further Mysteries of Ratio Deco Revealed
Are you able to calculate your decompression for a 40-50m/130-165 ft dive using only your average depth and bottom time? Here British techmeister Rich Walker further divulges the enigmatic mysteries behind GUE’s ratio decompression protocols in this part two of the series.
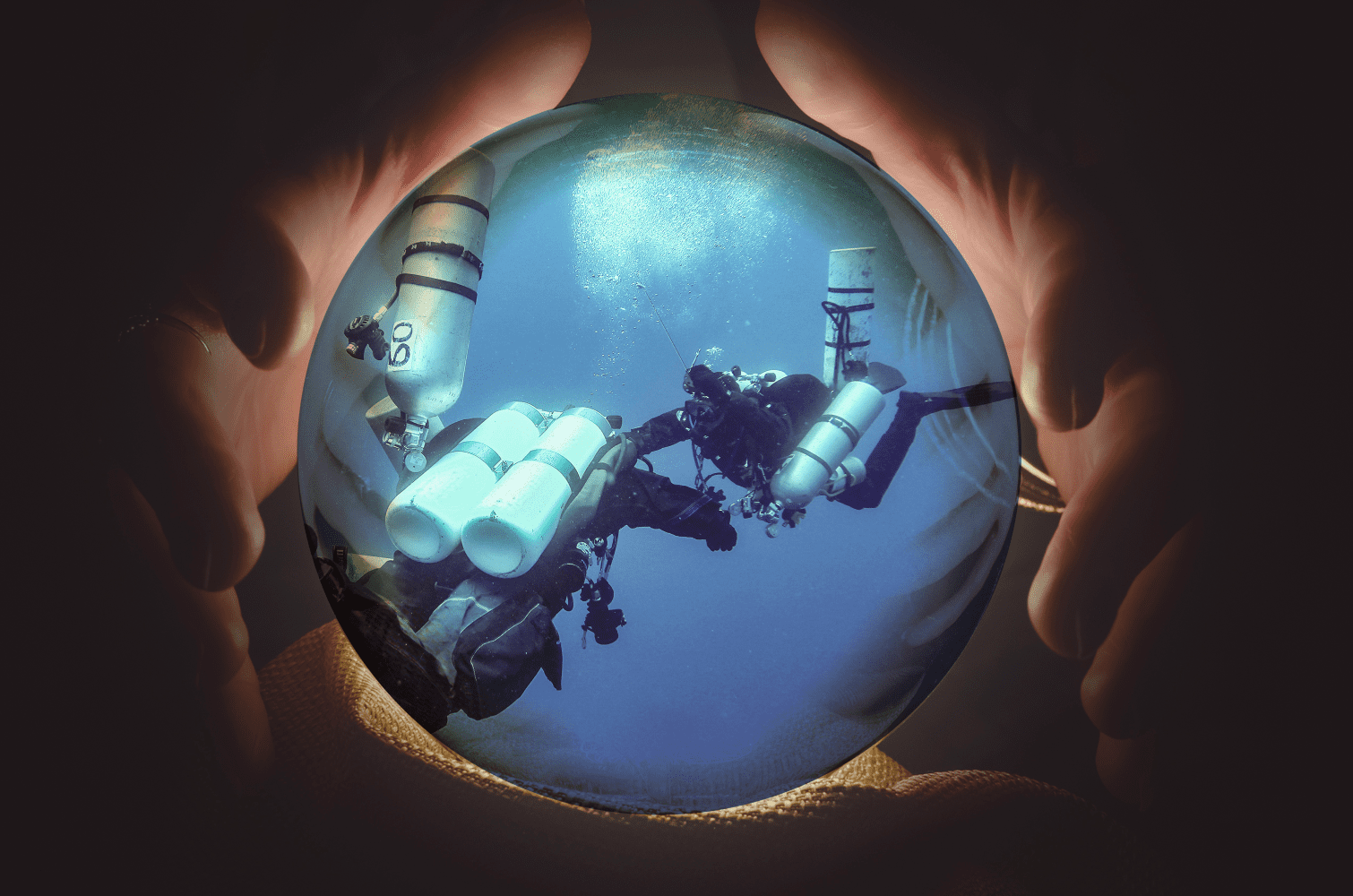
by Rich Walker
Header image original photo by Derk Remmers, edit by Amanda White
For Rules of Thumb-Part One see: Rules of Thumb: The Mysteries of Ratio Deco Revealed
In my last article, I explored some simple strategies you could use to calculate your no-decompression limit (NDL) and how much decompression time you needed if you went beyond that limit. That information applies to dives shallower than 30 m/100 ft. In my own diving, the tools are hugely valuable. I don’t need an expensive dive computer, or a powerful tool for cross-checking a computer if Santa dropped one down my chimney at Christmas.
But, I can hear all of you hardcore technical hipsters now:
“Yeah, but…”
My favourite words! But, it’s probably a fair question. Is there a way to work out decompression requirements in the 30-50 m/100-170 ft range? It would be a pretty short article if the answer were no.
Now, when we looked at the shallower strategies, we began by working out the NDL. To be honest, in the 30-50 m/100-170 ft depth range, there is no NDL that makes a dive worthwhile. If you’re happy with a 10 minute bottom time, then fill your boots. It takes me a good half an hour to even work out what day it is every morning, so I see little point in getting all dressed up for 10 minutes of working out where I am, realising that it might be a nice wreck, and then having to start the ascent.
So let’s not bother with NDL in this range. There might be one, but it’s not useful. In my last piece, I shared some tables that were generated from Global Underwater Explorers’ (GUE) DecoPlanner, using gradient factors of 100/100. I’m adopting a similar tactic now, but I’ll be using GUE’s default values of 20/85 gradient factors.
“Yeah, but…”
I know. Simon says. I’m not going to get into the merits and detriments of gradient factors. But, if you think that changing 20 GFLo to 30 or 40 is going to make a big difference, then run the tables and see the spectacular 3m/10 ft difference in the first stop depth and the whopping 1-2 minute change in decompression times. And, that all assumes you ascended at exactly 9 m/30 ft/min.
Okay, back to the topic after being so rudely interrupted.
Table It
Our depth range is past the point where nitrox has any significant benefit, and that air gas would likely blur my vision, so let’s use a trimix of 21% oxygen and 35% helium, or 21/35. We already know that we’re looking at decompression dives, so we’re also going to add a simple nitrox 50% for the shallower phases of the dive to help with off-gassing. We’ll switch to that gas at 21 m/70 ft.
The table, generated by Deco Planner, shows the decompression time required for each bottom time at each depth. I’ve given you a minute at 21 m/70 ft to get your gas switch done, and I’ve also ignored any decompression deeper than the gas switch. Typically, this is 1 minute or so at 24 m/80 ft for longer dives. This stop is usually done automatically as you slow down your ascent rate (you are ascending at 9 m/30 ft/min right?) as you approach the gas switch.
Anyway, let’s find some patterns in this pile of numbers. I’ve highlighted one interesting point—the 30 minute bottom time at 45 m/150 ft. Here, the bottom time is equal to the decompression time. If we look at the 25 minute dive, we can see that the decompression time is 23 minutes, so if we did the same decompression as the bottom time, then we’d be on the conservative side. The same is true of the 20 minute bottom time. If we did 35 minutes of decompression on the 35 minute dive, we’d be 2 minutes short. The first thing to note is that decompression time does not increase in a straight line—but I never said it did. I’m trying to force a simple straight line rule onto a curve, and that will have limitations. And a man’s got to know his limitations.
“Yeah, but…”
Of course. We need to look at what happens at different depths as well. If we start at our original point, 30 minutes at 45 m/150 ft, and go 3 m/10 ft shallower, the decompression time is 4 minutes shorter. Go one step shallower, and we get another 4 minutes shorter. So, maybe a simple and conservative rule might be to say, “If we are 3 m/10 ft shallower than the 45 m/150 ft depth, then we get 5 minutes less decompression than the bottom time.” There are a whole 35 different boxes to evaluate in the above table, so it’s worth laying out that analysis now.
The basic rule we’re trying to test is this: At 45 m/150 ft, total decompression time is equal to the bottom time. For each 3 m/10 ft shallower, we can say that the decompression time is 5 minutes shorter than the bottom time. The table below shows the real decompression requirement, our estimate as well as an error figure to see where the limitations lie.
Each of the boxes corresponds to an individual depth and time, and in each box there are three numbers. The real decompression in the center, the prediction of the simple rule in the bottom right, and the error in the top left. A negative number indicates missing decompression using the rule. A positive number indicates a conservative estimate. I also stopped calculating when the error became more than 5 minutes, hence the bottom right of the table is missing. The limitations are starting to appear.

More Detailed Analysis
Now, the sharper amongst you will notice that in the top left areas of the table, there seems to be a lot of red. This is particularly apparent when the predicted decompression is zero. But, let’s face it; any dive involving a gas switch to 50% is going to involve a slow-down and some sort of “safety stop.” Indeed, if you were to slow the ascent from 21 m/70 ft to a comfortable 3 m/10 ft/min, and then make a 5 minute safety stop at 6 m/20 ft—as recommended by your friendly local dive instructor—then the smallest practical decompression you could make would be 10 minutes. A minute at each stop from 21 m/70 ft to 9 m/30 ft, and then 5 minutes at 6 m/20 ft.
The rest of the table follows a more predictable pattern, but any estimated decompression longer than 30 minutes tends to get a little inaccurate. If the estimate is 30 minutes or less, then you are within a few minutes of the true figure. I’ve redrawn the table to reflect the “minimum decompression” and removed all dives with longer than 35 minutes of estimated decompression.
Now there are lots more green numbers, and the red numbers are smaller. We’ll get to the deeper depth shortly, but let’s finish up this job first. We’ve developed a simple rule, with some limitations, that allows us to estimate the amount of decompression we need to do for a given depth and bottom time.
What we haven’t done is examine how that decompression is organised in the water column. My method is driven by practicality, as well as a little religion. The way I do it is like this.
I know that the longest stop will need to be done at 6 m/20 ft, and that the rest of the time should be spent distributed across the 21-9 m/70-30 ft stops. I find that the easiest way is to simply divide my estimate of the total decompression by two, and spend that amount of time on the 6 m/20 ft stop.
I then divide the remainder equally across the intermediate stops. So, a 30 minute decompression would be 3 minutes at 21, 18, 15, 12 and 9 meters (/70, 60, 50, 40, and 30 ft) and then 15 minutes at 6 m/20 ft. A 20 minute decompression would be 2 minute stops and then 10 minutes at the final stop, and a 10 minute decompression would be 1 minute stops and a 5 minute final stop.
“Yeah, but…”
You’re right, 25 minutes of decompression and just about every other number gets clunky on the divisions, particularly for the intermediate stops. So, I standardise my decompressions to be one of three simple possibilities: 1’s and 5, 2’s and 10, or 3’s and 15. I calculate my decompression estimate based on the bottom time and average depth of the dive and pick the decompression schedule that fits, and round up to the next schedule if I end up in-between. I’m all for an easy life.
Now there’s no wetnotes full of tables. Just three different decompression schedules—pick 10, 20, or 30 minutes of decompression.
I mentioned religion a few lines back, and there is a school of thought that says that dividing the decompression by two to work out the final stop is a bit aggressive, and that it should be more like two thirds on the final stop. Technically, it’s right: and, indeed, on longer and deeper dives, this will work better. But for dives in this range, the simple split works very well.
Extending The Tool A Little Deeper
Now, I promised you a tool that would work to a depth of 51 m/170 ft, and so far we’ve only got to 45 m/150 ft. So, let’s finish off the tool. First, we’re going to switch to a different gas. Trimix 21/35 is a little light on the helium for dives past 45 m/150 ft (END >3.6 ATA), so an 18/45 is a better choice. The nitrox 50% is still a good choice for a decompression gas though.
We can follow a very similar approach to what we did above:
If we try our estimate strategy—but, instead of subtracting 5 minutes of decompression from the bottom time, we add 5 minutes to our estimate for every 3 m/10 ft deeper than 45 m/150 ft—we see that things are actually quite conservative. Here’s the full error table.
Note: The middle number represents predicted total decompression time from Deco Planner; the lower right the estimated decompression using the rule, and the upper left, the difference between the tool (green is greater, red is less)
Green figures all round! I’ve not calculated past 30 minutes of estimated decompression since we’d already established that as a limit.
So, we can finish off our complete rule for estimating decompression requirements for dives in the 33-51 m/110-170ft range.
- For a dive at 45 m/150 ft, the total decompression time is equal to the bottom time.
- For each 3 m/10 ft shallower than 45 m/150 ft, subtract 5 minutes from the bottom time to get the decompression time.
- For each 3 m/10 ft deeper than 45 m/150 ft, add 5 minutes to the bottom time to get the decompression time.
When you’ve worked out your total decompression time, pick one of the three schedules:
These tools are based on 21/35 trimix or 18/45 trimix for the bottom phase and nitrox 50% for the decompression. You can use other gases for sure, but it’s best to run the numbers through decompression planning software and make sure the rules work. And if they don’t, with a bit of work, you’ll find a strategy that does.
“Yeah, but…?”
For Rules of Thumb-Part One see: Rules of Thumb: The Mysteries of Ratio Deco Revealed
Dive Deeper:
InDepth: Standard Gases: The Simplicity of Everyone Singing the Same Song by Richard Walker
InDepth: Maintaining Unit Cohesion by Richard Walker
InDepth: Decompression, Deep Stops and the Pursuit of Precision in a Complex World by Jarrod Jablonski
InDepth: Part Two: Tech Divers, Deep Stops, and the Coming Apocalypse by Jarrod Jablonski

Rich Walker learned to dive in 1991 in the English Channel, quickly developing a love for wreck diving. The UK coastline has tens of thousands of wrecks to explore, from shallow waters to deep technical dives. He became aware of GUE in the late 1990s as his diving progressed more into the technical realm, and he eventually took cave training with GUE in 2003. His path was then set, and he began teaching for GUE in 2004.
He is an active project diver, and is currently involved with the Mars project (Sweden) and the cave exploration team in Izvor Licanke, Croatia. He is the Chairman and founder of Ghost Fishing UK. He is also a full time technical instructor and instructor evaluator with GUE, providing these services via his company, Wreck and Cave Ltd. He sits on GUE’s Board of Advisors and serves several other industry organizations.